The Art of Questioning - PQRST
In the previous article we looked at SAMPLE as a useful, but broad, tool for questioning the casualty as a means to assessing and diagnosing illnesses and injuries. PQRST is an acronym specifically for the assessment of Pain.
Pain is the most common symptom causing patients to seek medical attention yet most training is primarily concerned with treating injuries and illness with hardly any time spent on how to manage or assess the pain itself.
In many instances correct treatment of the injury or illness will reduce pain as a consequence; cooling a burn, stabilising a joint injury or correctly positioning a casualty with chest pain, for example, will in effect reduce pain as well as correcting the cause for concern.
Sometimes the cause is not obvious. Sometimes the casualty just presents with ‘pain’. No apparent injury, no history of illness. How do you treat that? What if definitive care is over 12 hours away, what do we do then?
Assessing Pain - PQRST
Pain is incredibly subjective and the term ‘pain’ is wildly vague. For the casualty to say “I’m in immense pain!” tells us nothing other than something is not normal. A critical, structured approach can help gather more detailed and relevant information:
Provocation
Sometimes the cause of the pain can be obvious; an injury or an existing medical condition. Sometimes there may be no obvious cause so look at what provokes the pain; what aggravates the pain or makes it worse? Movement of a joint, holding a particular position, coughing, laughing or deep breathing? If you can understand the mechanisms which aggravate the pain, maybe the source of the pain can be more accurately pinpointed.
Quality
Pain is a remarkably broad term so ask the casualty if they can you describe the pain: Is it a dull ache, a sharp stabbing pain, a vice-like gripping pain or a numb, tingling pain.
As a rule, neuralgic pain tends to be sharp and focused where as nociceptive pain from an injury can be more diffuse, depending on the mechanism of injury, the type of injury and the amount and type of tissue affected.
Chest pain could either be a serious sign of a cardiac condition or it could musculoskeletal if they have sustained trauma to the chest or strained muscles from exercise in the previous day or two.
Abdominal pain is always a cause for concern.
Radiates or Refers
A radiating pain spreads form the source of the pain. A referred pain is felt in a different location to the source of the problem.
Both of these phenomena are due to the nerves which are affected.
Radiating Pain
A classic example of a radiating pain is sciatica - the sciatic nerve is being pinched, usually in the lower spine or near the hip, which sends a signal to the brain indicating an issue but the signal does not reveal the exact location, as a result the pain is 'felt' down the leg, even as far as the big toe in some cases.
Referred Pain
A referred pain is felt in a different location of the body to the source of the problem. Nerves radiate out from the spine, separating into dendritic branches. At each junction - or ganglion - the nerves separate, leading to different areas. Pain felt by one nerve will send a signal to the brain, along the branches but the brain is sometimes confused as to which branch the signal came from and thereby misinterpreting its source.
The most common phenomena is "Brain freeze" when eating ice cream: The nerves at the palatine bone (the roof of you mouth) send a signal to the brain saying "The roof of my mouth is cold". These nerves share the same nervous pathway as the nerves that lead to the sphenoid bone which part of the front of the skull. The message received by the brain is "The front of my head is cold!" (so the next time you have brain freeze, you don't. You have sphenopalatine ganglioneuralgia).
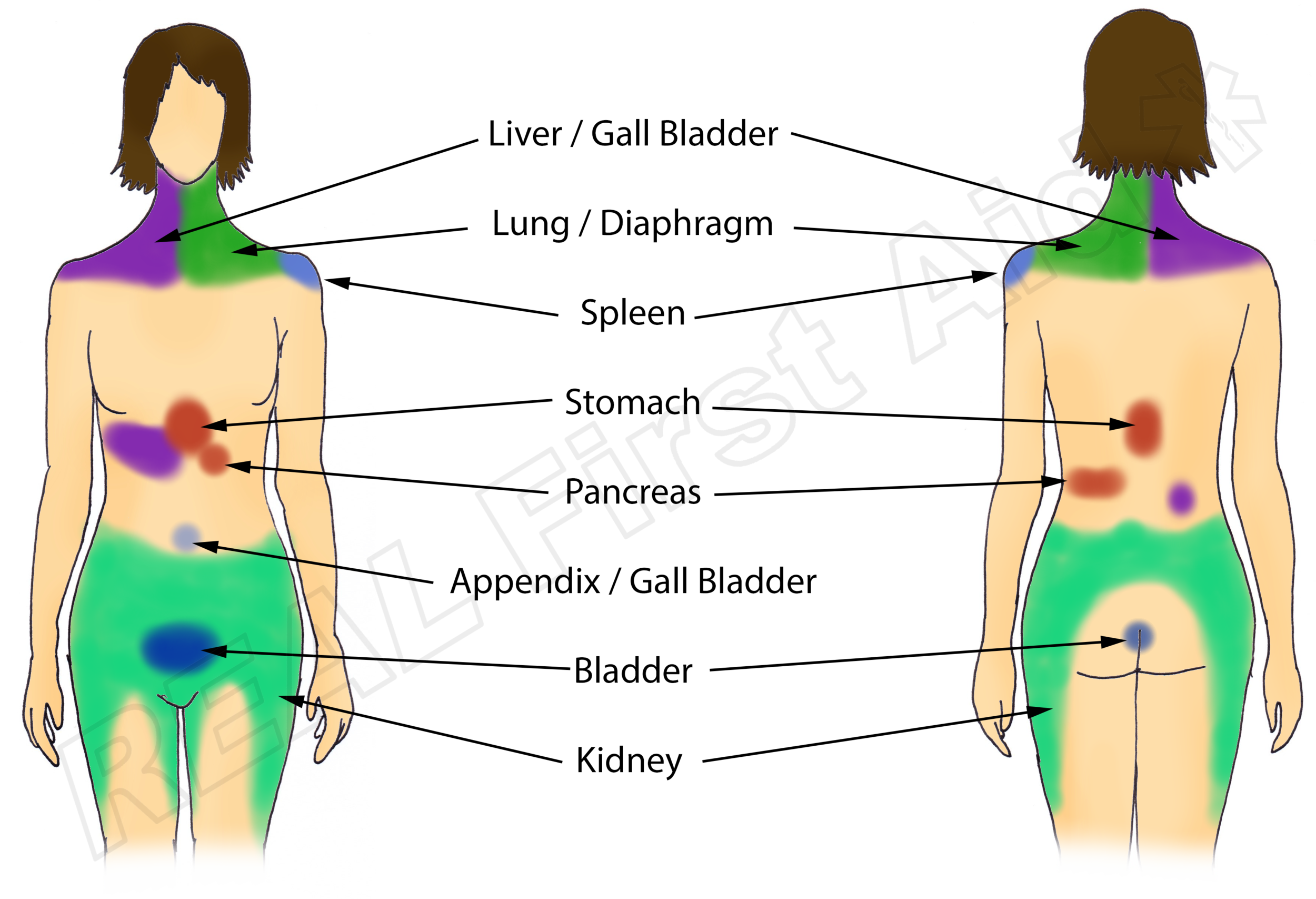
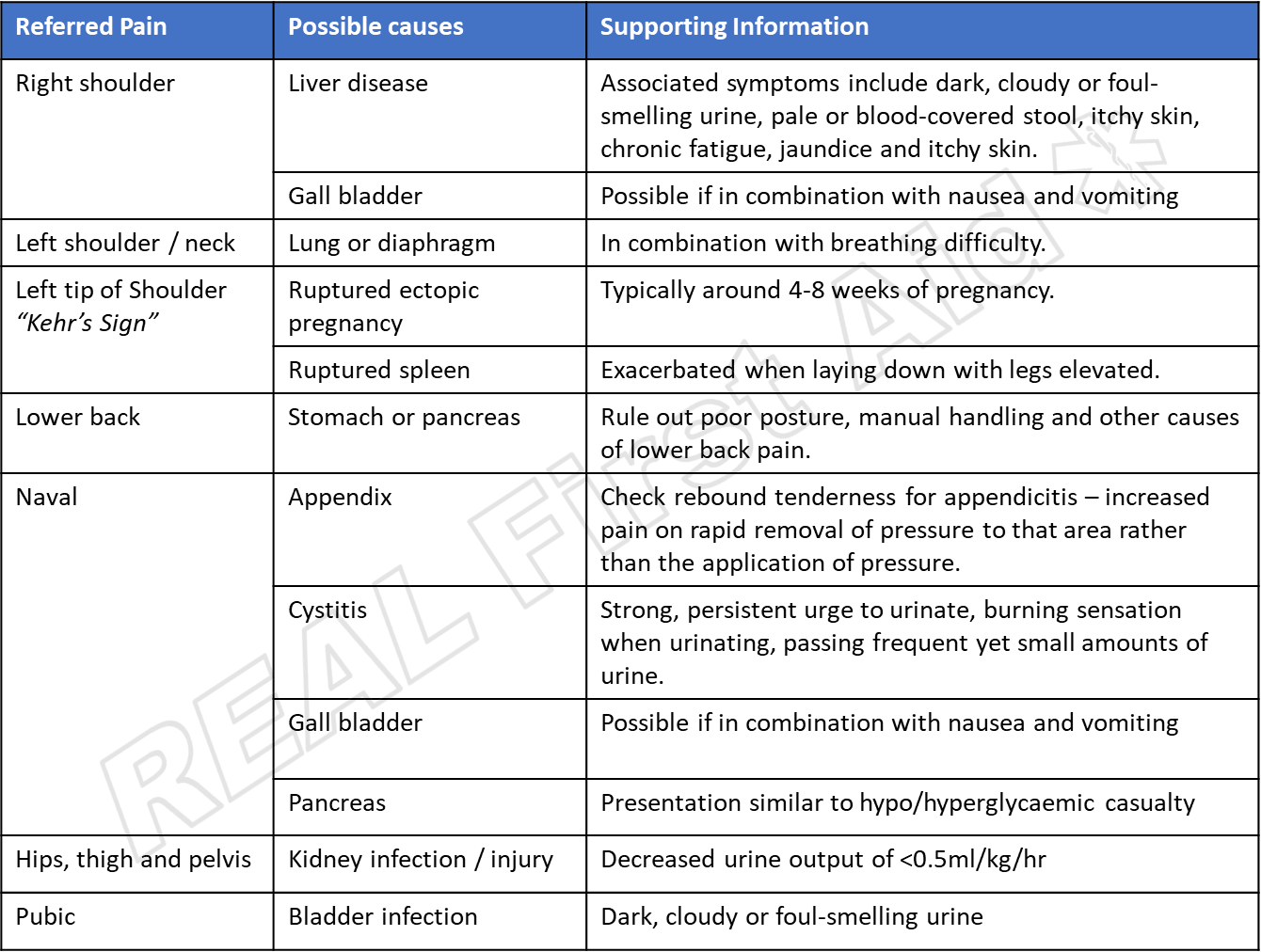
When assessing a casualty with pain, issues with certain organs may present as pain in seemingly random areas:
Severity
Because pain is so subjective, to describe the severity is practically worthless; a paper-cut can be agony to one person or a mild annoyance to another. A more useful assessment would be to ask the casualty to score the pain out of 10 (10 being the worst possible pain imaginable). This again is a subjective value on its own but if this question is repeated later on, a change in the value stated will indicate whether the pain is increase or getting better.
This is particularly useful
- if dealing with casualty’s for an extended period of time
- as an assessment of the efficacy of your treatment or pain medication
- as a means to mapping when the pain is worse.
Which brings us to ....
Time
When did it start? Is the pain constant or does it come and go? Is it worse at different times of the day?
The answers you get may enable you to make an informed decision or they may not mean anything to you. Whether you understand the answers or not they will mean something to someone, as such all communication is documented and handed over to definitive care.
Further Reading - Pain Management
Further Reading - The Medicine Cabinet