Part 3 - Screening Employees & Visitors
13th May 2020
A common question we have been asked is whether employees and visitors should be screened before arrival at a place of work?
The short answer, in our opinion, is No.
Returning to Work
On Sunday 10th we saw the beginning stages of the current Covid-19 social distancing measures begin to loosen as, in England, those who are not able to work from home are encouraged to return to work if it is safe to do so from Wednesday 13th May.
The Government on Monday 11th released 8 Practice Guidelines for certain business sectors to help them become ‘Covid Secure’.
Notably, whilst routine screening has been seen in airports and other areas, routine screening is not part of the suggested policies and practices.
The problems with Screening
When members of SAGE were asked about testing in the early stages of the outbreak two key words were repeatedly used – antigen and antibody
Antigens
An antigen is a toxin or other foreign body which triggers an immune response in the body, especially antibodies. By detecting viral antigens, which will be present in the body before antibodies form or symptoms of the disease are present, the tests can tell whether or not someone has the virus very early on regardless of if they are symptomatic or not.
Antibodies
Antibodies are produced in response to exposure of an antigen. An antibody test tells us what who has been infected but not if they are currently infected, because the antibodies are generated after a week or two by which time the virus should have been cleared from the system. It may, however, help track the spread of an infectious disease.
At the moment the majority of the current Covid-19 tests that all the reports are coming from are antigen tests using polymerise Chain Reaction (PCR) – collected from a swab at the back of the nose / throat - which detect the virus. This method relies on laboratory analysis which is time consuming and costly. The reason for this high cost and time consideration is due to two further terms which are also frequently referred to regarding testing- sensitivity and specificity
Sensitivity
Sensitivity is how accurate a test is at detecting the element being observed. Will the test identify very small traces of the antigen or will it only detect the antigen in large quantities.
Specificity
Specificity is how confident that the element being observed is what is believed to be observed. Is what you have identified specifically Covid-19 or could it be any other coronaviras, including the common seasonal flu?
Certain people can apply for Covid-19 Antigen testing using the .Gov website: https://www.gov.uk/guidance/coronavirus-covid-19-getting-tested
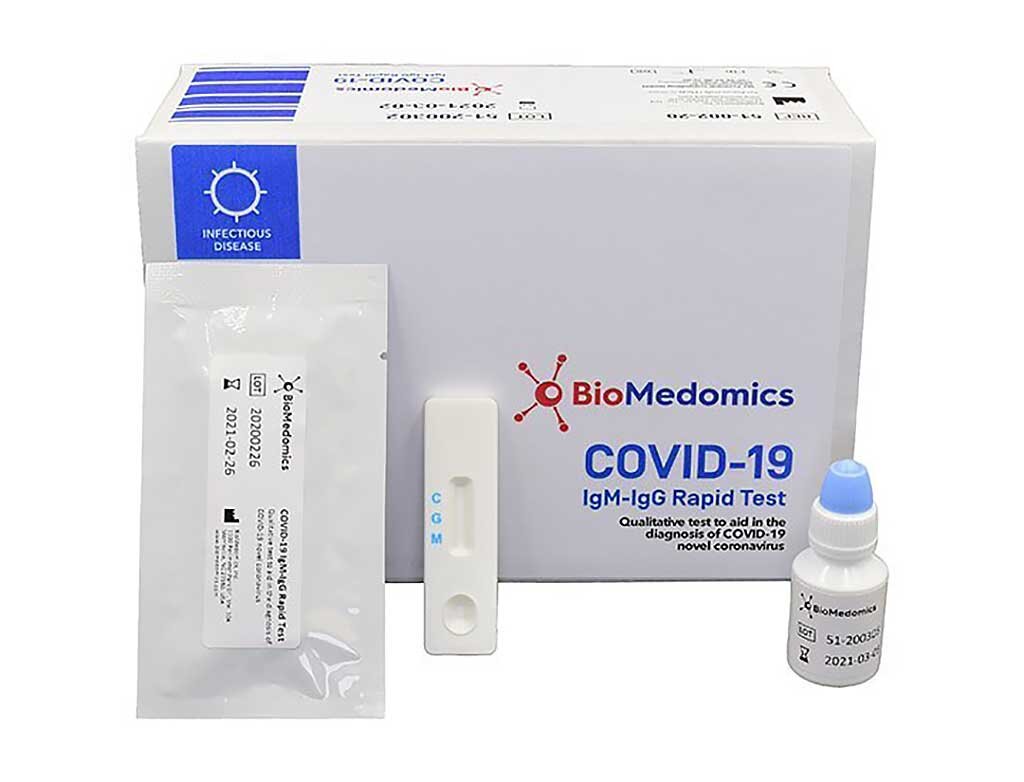
Rapid Diagnostic Tests
Several commercial companies are selling Rapid Dignostic Tests which can be performed in the workplace, provide almost instant results without the need for laboratory testing and analysis; the pregnancy test is a common example of a RDT.
Based on experience with antigen RDTs for other respiratory diseases such as influenza, the specificity of these tests might be expected to vary from 34% to 80%.1
One such company is AlphaBiolabs which currently retail at £60.00 +VAT per test. This should be done for every staff member, every day. Do the maths.
Because of the lack of both sensitivity and specificity another company, Regenerus Labs, has recently recalled its entire stock.
As for antibody testing, the majority of patients develop antibody response only in the second week after onset of symptoms (2-9). This means that a diagnosis of Covid-19 infection based on antibody response will often only be possible in the recovery phase, when many of the opportunities for clinical intervention or interruption of disease transmission have already passed. Antibody detection tests targeting Covid-19 may also cross-react with other pathogens, including other human coronaviruses (10-12) and give false-positive results.
There has been discussion about whether RDTs detecting antibodies could predict whether an individual was immune to reinfection with the Covid-19 virus however there is no evidence to date to support this.
As such we DO NOT recommend Rapid Diagnostic Tests for workplace screening.
Temperature testing
Early on, a fever of 38oc or over was considered an indicator of Covid-19. Temperature testing is very sensitive - with infrared (IR) thermometers being able to detect temperature to +/- 0.1oc - but it is not specific;
An elevated temperature is not specific to Covid-19, it could be caused by other factors as simple as exercise or ambient temperature. These factors would needed to be understood by the person conducting the screening process and a judgment call would need to be made.
Combined with the estimate that as many as 70% of carriers of Covid-19 may not display an elevated temperature (13) temperature sensing may only detect only 50% of all cases (14).
As such we DO NOT recommend temperature testing for workplace screening.
Workplace Testing leads to Complacency
Picture the scene.
Your employee is symptomatic - they don’t feel well so, correctly, stay at home and self isolate.
Another employee claims to be asymptmatic - they feel fine so decide to come to work. If they are tested at the door and found to have a high temperature, they are sent home. This is a good thing as you have ruled out a probable carrier.
If they have been tested at the door, found not to have a high temperature they are allowed in to work.
There is a 50% chance they are still carrying the infection but in their mind they have been 'cleared'. They have seen people being turned away. They are now in a workplace where everyone else also believes that they are also ‘clear’ because they have been tested and allowed in.
Among the workforce, the general belief is that no one in work has Covid-19. If anything, the workforce are in a 'clear' zone, the safest place they can be, unlike the supermarket or garden centre where no one is tested as they come in.
Where is their motivation to obey the Social Distancing and other measures the employer has put in place? And we know how humans behave when they think they are safe.
If we work on the assumption that no one can be completely clear, it leads to caution.
Recommendations
We have a legal duty of care to provide a safe and healthy environment for all employees and visitors, as such follow the Government guidance provided to reduce the risk of spreading the disease by implementing social distancing measures and other practicable measures to your processes and operations.
Provide additional training and signage so that your employees and visitors are aware of their obligations to reduce the spread of the infection.
Once this can be effectively implemented should employees be encouraged to return to work where they cannot work from home.
Anyone who is symptomatic, or cohabiting with someone who is symptomatic, should not be in work.
Assume everyone at work, who is asymptomatic is infected.
Assume every visitor who is asymptomatic is infected.
Working on the assumption that everyone is infected is the best way to reduce the likelihood of transmission whilst continuing with business operations.
References
Bruning AHL, Leeflang MMG, Vos JMBW, Spijker R, de Jong MD, Wolthers KC, et al. (2017) “Rapid Tests for Influenza, Respiratory Syncytial Virus, and Other Respiratory Viruses: A Systematic Review and Meta-analysis”. Clinical Infectious Disease. Sep 15
Liu Y, Liu Y, Diao B, Ren Feifei, et al. (2000) “Diagnostic indexes of a rapid IgG/IgM combined antibody test for SARS-CoV-2”. Medxriv. https://doi.org/10.1101/2020.03.26.20044883
Zhao J, Yuan Q, Wang H, Liu W, Liao X, Su Y, et al. (2020) “Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019”. Medxriv. https://www.medrxiv.org/content/10.1101/2020.03.02.20030189v1.full.pdf
Okba N.M.A, Muller M.A., Li W, Wang C, et al. (2020) “SARS-COV-2 specific antibody responses in COVID-19 patients”. Medxriv. https://www.medrxiv.org/content/10.1101/2020.03.18.20038059v1
Wölfel R, Corman V, Guggemos W, Seilmaier M, Mueller M, Niemeyer D, et al. (2020) “Virological assessment of hospitalized patients with COVID-2019”. Nature. https://www.nature.com/articles/s41586-020-2196-x
Lou B, Li T, Zheng S, Su Y, Li Z, Liu W, et al. (2020) “Serology characteristics of SARS-CoV-2 infection since the exposure and post symptoms onset”. Medxriv. https://www.medrxiv.org/content/10.1101/2020.03.23.20041707v1.full.pdf
Liu W, Liu L, Kou G, Zheng Y, et al. (2020) “Evaluation of nucleocapsid and spike protein-based ELISAs for detecting antibodies against SARS-CoV-2”. Medxriv. https://doi.org/10.1101/2020.03.16.20035014
Zhang W, Du R, Li B, Zheng X, et al. (2020) “Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes”. Emerging microbes and infections. 9(1):386-389.
Zhou P, Yang XL, Wang X, Hu B, et al. (2020) “A pneumonia outbreak associated with a new coronavirus of probable bat origin”. Nature. Mar; 579(7798):270-273
Okba N.M.A, Muller M.A., Li W, Wang C, et al. (2020) “SARS-COV-2 specific antibody responses in COVID-19 patients. Medxriv. https://www.medrxiv.org/content/10.1101/2020.03.18.20038059v1
Wang N, Li SY, Yang XL, et al. (2018) “Serological Evidence of Bat SARS-Related Coronavirus Infection in Humans, China”. Virologica Sinica. 2018;33(1):104–107.
Che X, Qiu L, Liao Z, Wang Y, et al. (2005) “Antigenic cross-reactivity between severe acute respiratory syndrome-associated coronavirus and human coronaviruses 229E and OC43”. The Journal of Infectious Diseases. 191(12). 2033–2037
Quilty, B. J., Clifford, S., Flasche, S., Eggo, R. M., & CMMID nCoV working group (2020). “Effectiveness of airport screening at detecting travellers infected with novel coronavirus (2019-nCoV)”. Euro surveillance: bulletin Europeen sur les maladies transmissibles. 25(5),
Richardson S, Hirsch JS, Narasimhan M, et al. (2020) “Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area”. The Journal of the American Medical Association. https://jamanetwork.com/journals/jama/fullarticle/2765184