Hypothermia
26th January 2014 revised 15th January 2019 and 30th November 2021
Prologue
Environmental Illnesses such as Heat Stroke and Hypothermia are entirely preventable. Casualties with either of these conditions are usually a result of:
Inappropriate equipment
Lack of education
Bad planning
These casualties should be those who you happen upon or are called to. No one in your group should ever be a casualty of environmental illness. Both heat illness and hypothermia should be exercises in prevention.
Physiology
The normal core temperature of a healthy adult is often cited as 37°C but a core temperature of anywhere between 36.5–37.5°C it is perfectly normal with variations due to age, gender, weight and how it is measured, for example (1). Some studies have even found oral measurements varying as widely as 33.2-38.2°C.
Hypothermia is defined as a core temperature of 35°C or less (2) and occurs when your body’s heat loss exceeds its heat generation, causing core temperature to drop. As this happens metabolic processes (including the use of chemical energy, heat generation, respiration) slow down. The body’s systems will eventually start to shut down with vital organs eventually ceasing to function.
We generate our own heat through metabolic processes and can further increase heat generation through physical exercise but both of these abilities are dependent on energy from food we have consumed. We can also reduce heat loss by vasoconstriction – the constriction of blood vessels shunting warm blood away from the skin towards the core - but can never fully prevent it.
In an ambient environment of 28°C the normal metabolic processes of a healthy person can maintain a normal core process whilst naked and motionless (3). We will be able to generate heat at the same rate that it is being lost to the environment. Unfortunately the mean surface temperature of the earth is around 14.6°C (4) meaning most people will be somewhere or at some time where they are losing heat to the environment.
Heat is lost by several mechanisms:
Radiation Heat emitted from a body when it is in an environment or medium at a lower temperature than it is.
Convection The transfer of heat from one place to another through the movement of air.
Conduction The transfer of heat from one body to another through direct contact.
Evaporation Heat loss in the form of energy transfer needed to vaporise water. Water does not need to boil to evaporate; evaporation will occur close to 0°C. Energy is needed to break the molecular bonds which come from the heat of the ambient air or the surface the water is in contact with. The greater the difference in temperature between the surface and the air, the greater the heat loss from the surface.
Respiration There are two heat losses in this process; the introduction of cold air during inhalation cools the core through convection and also as moisture inside the lungs is evaporated and exhaled.
Stages of Hypothermia
Hypothermia is categorised in stages determined by core temperature. We are not able to measure core temperature accurately in a pre-hospital setting without a thermometer.
Avoid the use of oral thermometers as glass thermometers are easily broken and it is not usually advised to place anything in a casualty’s mouth, especially if they have a reduced level of consciousness unless it is used to secure the airway.
A tympanic (ear) thermometer is accurate and easy to use but expensive and bulky. Perhaps most importantly, as tympanic thermometers are typically used to identify fever, they do not tend to record temperatures below 34oc, where they just display “Low”. This is wholly inappropriate for a hypothermic casualty.
Cheap digital refrigerator thermometers can be used to measure axillary (armpit) temperature. The non-invasive wired probe can remain in place while the display is left on the outside of the packaged casualty allowing constant monitoring without having to undress or expose the casualty.
Axillary temperature is typically 35.5-37.0°C (5) or in other words, up to 1.5°C less than the cited core mean temperature. Temperature correlation is not particularly accurate but even a cheap digital thermometer will show change over time. As the ambient temperature will affect everyone, the sense of touch will not be accurate enough to detect temperature change at low temperatures.
* References 6-8
To warm or not to warm?
There is confusion about how quickly a hypothermic casualty should be warmed and by what methods. As hypothermia progresses, the casualty will lose metabolic functions to the point of irregular heart rhythms and even cardiac arrest. Aggressive warming or rough handling of the casualty can, in some cases lead to Ventricular Fibrillation and even arrest. (9, 10)
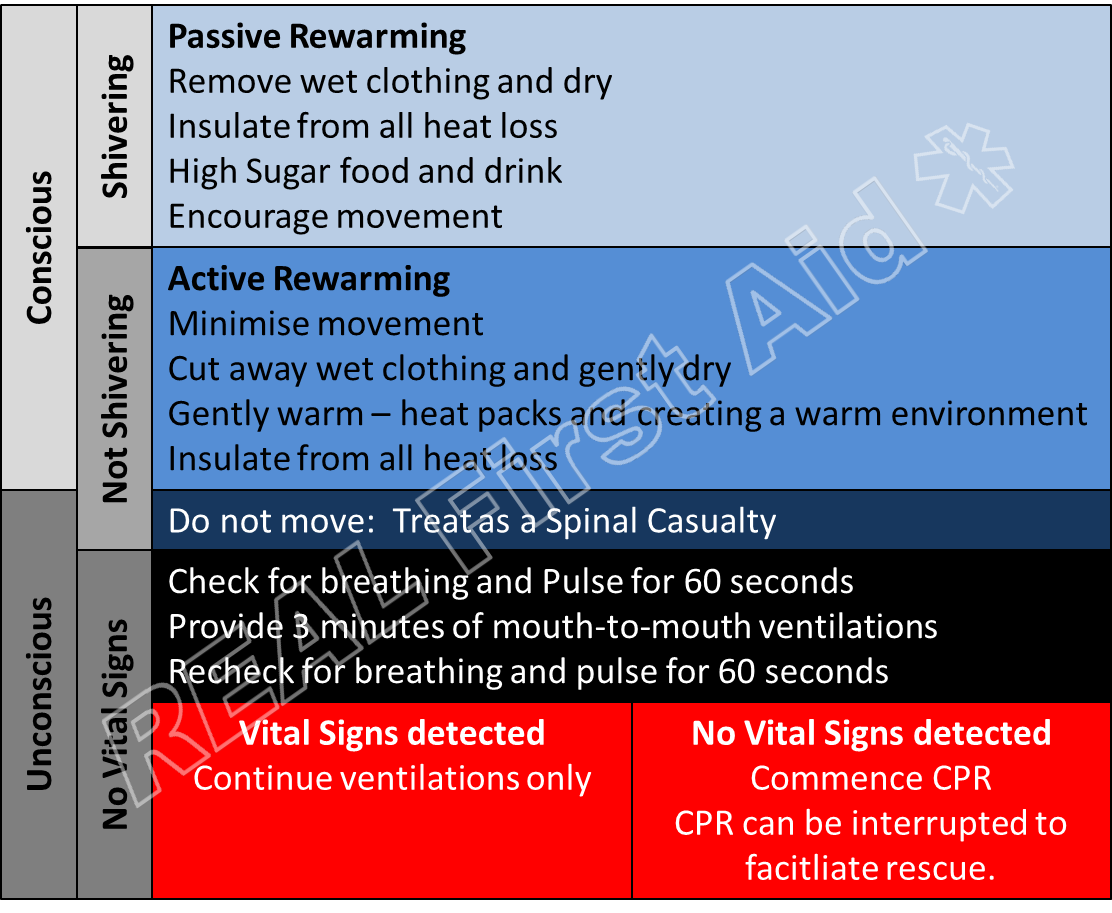
The management of a hypothermic casualty is determined by the stage of hypothermia they are exhibiting. As it can be difficult, or at all possible, to accurately measure core temperature in the field a more practical approach may be to treat according to exhibited behaviours.
Does hot food and drink help rewarm casualties?
The temperature of the food or drink makes almost no difference in the casualty’s core temperature (11). This is simple physics; if you imagine a healthy adult male weighs 100kg, this is the same weight as 100 liters of water, which is approximately the same as half a bathtub filled with water. If you were to half fill a bath with water at 36oc adding a hot cup of tea to the water will have an almost negligible effect to the temperature of the water.
The casualty is craving glucose which is required to shiver or exercise - both of which raise core temperature. The temperature of the food or drink is only of psychological benefit. A cold bottle of high-sugar soft drink would have much more effect on the rewarming process than the same volume of hot tea or coffee (assuming no sugar is added). But the psychological effect cannot be ignored completely and hot cordials have great success in providing energy and morale in cold casualties. Ribena is a personal favourite.
Mild Hypothermia
The casualty is conscious and shivering. This is normal; the casualty is Little Sick. The casualty is mildly hypothermic but has not lost the normal metabolic processes needed to generate heat.
Heat is primarily generated in muscle tissue; shivering and exercise can increase heat production 2 to 4 fold.(12) Surface warming (heat packs, skin-to-skin contact etc) inhibits shivering heat generation (6) so other than the feeling of warmth against the casualty’s skin, there is no net heat gain in applying external heat to an actively shivering, mildly hypothermic casualty. As they are generating heat themselves (spontaneous rewarming), the most effective method to raise core temperature is to reduce heat loss by insulating and ensuring they have enough energy to continue generating heat.
Convection: Provide shelter from the wind (Group shelter, ‘space blanket’, tarp, flysheet etc.)
Evaporation: Remove all wet clothes.
Radiation: Replace with dry clothes.
Energy: Provide high sugar food and drinks if tolerated: Without calories the casualty will lose the ability to shiver. Sugary drinks are metabolised quicker than foods. (Hot sugary food or drink would be ideal but at this stage the sugar is more important than the food or drink being hot)
Exercise: The best way to cool down is to sit still so employ the above measures as quickly as possible and then keep moving. Food and drink must be provided before exerting the casualty otherwise the casualty may exhaust their energy stores and deteriorate.
Moderately Hypothermia
This casualty is cold but not shivering. This is not normal; the casualty is Big Sick. As the casualty is not generating their own heat (spontaneous rewarming) we must raise their temperature, but carefully. This is Active Rewarming.
As we can generally only warm casualties from the outside-in (e.g. through the skin) there is a long held theoretical fear that warming the casualty will promote vasodilation – opening of the blood vessels at the skin – and subsequent reduction of blood pressure and reduced perfusion to the vital organs. Other than immersing the casualty in hot water, this appears to be unfounded (6) but rough handling may trigger ventricular fibrillation. As such the casualty is insulated to prevent heat loss and warmed without unnecessary movement.
Convection: Provide shelter from the wind. (Group shelter, survival bag, tent etc.)
Related article: Packaging Hypothermic CasualtiesEvaporation: Remove all wet clothes – cut off to avoid movement
Radiation: Insulate to prevent radiative heat loss (sleeping bag, duvet jackets etc)
Conduction: Insulate underneath the casualty (sleeping mats etc.)
Direct Heat: Apply chemical heat packs to the armpits, groin and back of the neck. (Water bottles filled with warm water are an effective alternative but must be periodically rewarmed). Heat packs should be covered (e.g. thick socks) to prevent burns.
Ambient Heat: Increase the ambient temperature (group shelter, huddling etc)
Do not exercise the casualty. Keep the casualty insulated but immobile.
If you suspect the casualty is at risk of becoming unconscious, do not make them drink or consume food because of the risk of compromising the airway with vomit in the unconscious casualty.
If the casualty is unconscious but with detectable vital signs, do not move the casualty – treat as a Spinal Casualty.
Severely Hypothermic
The casualty will be unconscious and appear dead. As the casualty deteriorates, vital signs such as breathing, blood pressure (e.g. a detectable pulse) and heart rate slow down to the point of being barely detectable. In a non-hypothermic casualty who is not breathing, we would ordinarily call for help and commence CPR. The severely hypothermic casualty is in a delicate balance. Aggressive movement of the casualty (including CPR) may actually trigger cardiac arrest (6, 8, 13).
Cooling reduces resting oxygen consumption of most human tissue by about 6% per 1°C decrease with a greater decrease in brain tissue. Hypothermia preferentially protects the brain from hypoxia. At a core temperature of 28°C. whole body oxygen consumption is about 50% of normal (13) whereas brain oxygen consumption can be reduced to about 35% of normal.(14) At very low core temperatures the brain can tolerate more than 30 minutes of circulatory arrest.(15,16)
The classic teaching is that CPR must be started promptly and continued without interruption until a return of spontaneous circulation (ROSC) can be established. This is not the case in patients with severe hypothermia: There are several cases of hypothermic casualties being successfully resuscitated – with normal neurological outcomes – after prolonged delays of up to 70 minutes (16) and intermittent CPR provided for one minute at one minute intervals (17).
The lowest known core temperature from which a patient with accidental hypothermia has been successfully resuscitated is 13.7°C. (18)
Check for vital signs for 60 seconds.
If vital signs cannot be detected, do not do CPR - provide mouth-to-mouth rescue breaths for 3 minutes (this may improve previously undetectable vital signs).
Recheck vital signs for 60 seconds.
Detectable Vital Signs (19)
Do not do CPR, continue rescue breaths. (A weak pulse in addition to rescue breaths may provide effective perfusion. If Ventricular fibrillation is inadvertently caused through CPR, this perfusion will be lost.)
No detectable Vital Signs (19)
In patients with severe or profound hypothermia, CPR can be delayed (“scoop and run”) and can be given intermittently during evacuation if it is not technically possible or safe to perform continuous CPR. Unlike conventional Remote CPR Protocols, CPR can be given for several hours, if necessary.
Immersion Hypothermia
The cause of death due to immersion in cold water immersion is rarely due to hypothermia but rather drowning.
Upon immersion in cold water, the initial shock causes a variety of problems:
A primordial ‘gasp reflex’ on immersion to cold water combined with hyperventilation and a difficulty in controlling breathing increases the risk of inhaling water. This is transient and lasts for approximately 3 minutes. This is the first thing that is likely to cause death. (6, 13)
If the casualty is able to control their breathing, their blood vessels by this point will have shunted warm, peripheral blood to the core, reducing blood flow to the limbs. In combination with a delayed motor response, swimming or ‘treading water’ becomes difficult even for a strong swimmer in cold water. The casualty is now at risk of drowning or exhausting themselves.
The least likely cause of death in Cold Water Immersion casualties is hypothermia. If the casualty has managed to control their breathing and not aspirate water immediately after immersion and managed to have remained afloat despite almost paralysis they will be losing heat but not as quickly as previously thought.
The internet is full of survival prediction models based on the duration of exposure and water temperature but these should largely be ignored in the pre-hospital setting:
The majority of popular models appear to be replicated because of their simplicity but have no cited evidence behind them. They are the equivalent of ‘old wives tales’ handed down and recited without any questioning.
The more robust models are incredibly complex and would be impossible to apply practically.
As with exposure hypothermia, the cold water immersion casualty should be treated based on exhibited behaviour.
Treatment Summary
Rather than worrying about the core temperature of the casualty or which stage of hypothermia they may be at, treat based on exhibited signs:
Post Care Issues
As the casualty recovers, de-escalate the treatment plan but monitor the casualty for deterioration.
After Drop
A phenomenon known as “After Drop” can occur as a result of aggressive rewarming; peripheral vasodilation can lead to a redistribution of blood and a drop in core temperature. This can occur during treatment or even after recovery. This can be prevented by moderated warming techniques; If the casualty has vital signs, is insulated and immobile, there is no rush to actively warm them.
Circum Rescue Collapse
Particularly evident in immersion hypothermia casualties, ‘Circum Rescue Collapse’ has been attributed to the aggressive repositioning of the casualty from a floating horizontal position to vertical as they were winched out of the sea using a hoist. Standing up quickly can cause orthostatic hypotension; a drop in blood pressure as the vascular system cannot constrict fast enough in the lower limbs and abdomen to squeeze oxygenated blood up to the brain; this is noticeable by the ‘head rush’ or feeling of light-headedness as the brain is momentarily deprived of oxygen. (It’s not a head rush, It’s a foot drain.)
Combined with the immediate loss of hydrostatic pressure which was being exerted on the body whilst the casualty was immersed, this drop in blood pressure can reduce cerebral perfusion to the point of unconsciousness and cardiac perfusion to the point of cardiac arrest.
Both immersion and severely hypothermic casualties are now rescued horizontally and as such, should remain in this position until rescue.
Epilogue
Environmental Illnesses affect everyone: If one member of your group is exhibiting signs of hypothermia, treat everyone in the group. If one person is hypothermic, everyone else is likely to become hypothermic as all members have been exposed to the same environment so they are all treated preemptively. Stop for as short a time as possible, take on more food and drink, recheck equipment (do up zips, get an extra layer on) and then get moving again.
Related Articles:
Packaging a Hypothermic Casualty
Heat Stroke & Heat Related Illnesses
Big Sick or Little Sick? 5 Basic Vital Signs
CPR in Remote Environments
Karakitsos D, Karabinis A (2008). "Hypothermia therapy after traumatic brain injury in children". The New England Journal of Medicine. 359 (11): 1179–80
Brown, DJ; Brugger, H; Boyd, J; Paal, P (2012). "Accidental hypothermia.". The New England Journal of Medicine 367 (20): 1930–8.
Wlkerson JA (Ed) (1998) Medicine for Mountaineering & Other Wilderness Activities. The Mountaineers. Seattle. p300
“NASA Finds 2013 Sustained Long-Term Climate Warming Trend”. Posted Jan. 21, 2014. Accessed Oct. 24 2014http://www.giss.nasa.gov/research/news/20140121/
Sund-Levander M, Forsberg C and Karin Wahren L. (2002) “Normal oral, rectal, tympanic and axillary body temperature in adult men and women: a systematic literature review”. Scandinavian Journal of Caring Sciences. Vol. 16 No. 2: 122
Geisbrech GG (2001) “Pre hospital treatment of hypothermia”. Wilderness and Environmental Medicine. 12, 24–31
Duff J, Gormly P(2010) First Aid and Wilderness Medicine. Cicerone Press. Singapore.
Department of Health and Social Services(2003) State of Alaska Cold Injuries Guidelines. Division of Public Health Section of Community Health and EMS
Golden FSC, Hervey GR, Tipton MJ. (1991) Circum-rescue collapse: collapse, sometimes fatal, associated with rescue of immersion victims. Journal of the Royal Navy Medical Service. 77:139–149.
Giesbrecht GG. (2000) Cold stress, near drowning and accidental hypothermia: a review. Aviation, Space and Environmental Medicine. 71:733–752.
Jones D Bowles J, Bergquist-Turori D, Cooper C, Rostomily K, Pautz C, Heaney J. (2020) “Evaluation of Three Field Rewarming Techniques During Cold Weather Military Training”. Wilderness and Environmental Medicine. 31(3). 285-290
Hanania NA, Zimmerman JL (1999). "Accidental hypothermia". Critical Care Clinics. 15 (2): 235–49
Danzl D. (2012) “Accidental hypothermia”. In Auerbach PS (ed) Wilderness Medicine 6th ed. Philadelphia. Elsevier. pp116–142.
Michenfelder JD, Milde JH. (1991) “The relationship among canine brain temperature, metabolism, and function during hypothermia”. Anesthesiology. 75:130–136.
Soar J, Perkins GD, Abbas G, et al. (2010) “European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution.” Resuscitation. 81:1400–1433.
Althaus U, Aeberhard P, Schüpbach P, Nachbur BH, Mühlemann W. (1982) “Management of profound accidental hypothermia with cardiorespiratory arrest”. Annals of Surgery. 195:492-495
Boue Y, Lavolaine J, Bouzat P, Matraxia S, Chavanon O, Payen JF. (2014) “Neurologic recovery from profound accidental hypothermia after 5 hours of cardiopulmonary resuscitation”. Critical Care Medicine. 42:e167-e170.
Gilbert M, Busund R, Skagseth A, Nilsen PA, Solbo JP. (2000) “Resuscitation from accidental hypothermia of 13.7 degrees C with circulatory arrest”. Lancet. 355:375-376
Zafren K. Giesbrecht GG, Danzl DF, Brugger H, et al. (2014) “Wilderness Medical Society Practice Guidelines for the Out-of-Hospital Evaluation and Treatment of Accidental Hypothermia: 2014 Update”. Wilderness and Environmental Medicine. 25, S66–S85
Mekjavić IB, La Prairie A, Burke W, Lindborg B. (1987) Respiratory drive during sudden cold water immersion. Respiration Physiology. 70(1):121-30.